I often get asked how ozempic dental side effects relate to their oral health. Below is a concise 3 point analysis for the issues it can cause on your mouth and 3 things I would recommend.
One common drug used today is Ozempic, known for weight loss. If these side effects are not addressed in time, the side effects can be catastrophic.
To those who ask if the effect has happened on their teeth, I almost always have to ask what they have noticed. Patients usually notice oral changes before I do. The most common side effects are not being able to speak without a bottle of water. Or they often wake up at night feeling very dry or having trouble speaking and eating.
I notice more patients using GLP-1 receptor agonists, such as Ozempic. The most common usage is for diabetes or weight loss. While it is important to address the health of the patient, patients need to be aware of the side effects. The impact on oral health is significant and all too often overlooked.
To begin, we first need to address the way these medications affect the body. Ozempic’s use shows a complex link between the drug, saliva, and oral health.
Issue #1 – Saliva is altered significantly.
Ozempic impacts oral health in two primary ways.
First, Ozempic reduces salivary flow by acting on GLP-1 receptors, causing dry mouth. When saliva decreases, bacteria have an easier time thriving. Saliva usually washes away food, neutralizes acids, and provides minerals to strengthen teeth. Less saliva means less natural protection against decay-causing agents. (1, 2)
Research shows that GLP-1 receptor agonists can lead to dry mouth. Their use increases the risk of bad breath, tooth decay, and gum disease. This is especially true when saliva is low, according to dental studies (3).
The second issue is just as serious. Even when saliva is made, GLP-1 agonists change the balance of proteins and electrolytes. This means, saliva loses most of its protective ability under prolonged use of Ozempic (4). Which is worse because now it isn’t as good but also less in quantity. Between these two factors, the stage is set for problems to take place.
Both issues are classic manifestations of ozempic dental side effects – which are usually observed on a clinical level.
Clinical Manifestations I Observe as a Dentist
These two problems, when compounded, show during clinical exams. After prolonged use, patients with medically induced dry mouth (5) show distinct signs. Their tongues often look smoother and more inflamed. Also, oral tissues are much drier than usual. In most patients, saliva pools accumulate during exams. However, this is missing in those with dry mouth from medication.
Clinical records support these findings. Patients with severe dryness have measurably different saliva. Testing is frothy in nature and less than normal amounts. The modified Schirmer test shows a mean of 9 mL at 3 minutes, with a range of 8-10 mL. This confirms that semaglutide can cause dry mouth, as noted in medical literature.
The technical side of things: (Skip this if you want – geeks like me, read on)
GLP-1 agonists, such as Ozempic, affect the nervous system that controls saliva production. This reduces key antimicrobial agents, including salivary immunoglobulin A (sIgA), lactoferrin, lysozyme, and peroxidase. The impact is significant, as sIgA is crucial for fighting oral pathogens. Less of it means that more pathogens can stick to the oral mucosa.
Ozempic’s appetite suppression adds another risk for oral health. Rapid weight loss leads to deficiencies in zinc, vitamin A, and vitamin D, all vital for oral immunity. This protein-energy malnutrition slows healing down and increases the risk of mouth sores.
GLP-1 receptors on immune cells complicate things further. The activation reduces inflammation but also weakens immune responses in the mouth. Data show that GLP-1 medications weaken mouth defenses. This makes fungal infections like oral thrush more likely. This causes painful sores on the tongue, gums, and cheeks, as reported in clinical observations.
Issue #2 – It’s not just saliva: Gastrointestinal Side Effects
Lack of saliva and its altered state isn’t the only problem when Ozempic is used. When one is using the drug, another common side effect is nausea or vomiting. Both the ‘spit-up’ (frequent with nausea) and the vomiting change the oral pH. This change makes the oral condition more acidic, thereby weakening enamel. Long exposure in these conditions can cause enamel failure and make oral problems worse.
These gastrointestinal effects create a perfect storm for dental damage. All the enamel gets destroyed over time. Low saliva can’t neutralize stomach acid, and changed saliva can’t remineralize teeth well. Being in this environment is like pouring battery acid on your car every day. Battery acid will eat through the hood over time. Ultimately, this will damage the motor and ruin the car. The same problem happens with your teeth. If chronic vomiting is an issue, the enamel ends up getting completely obliterated causing significant issues in the future.
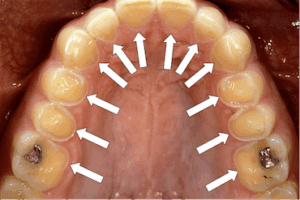
Erosion-from frequent vomiting will be seen if vomiting keeps happening for extended periods of time. The enamel is destroyed from the acidic insult.
Issue #3 – Facial Structure Changes and Long-term Considerations
While much less immediate, long-term effects should be taken into consideration. On a positive note, rapid weight loss will change facial structure. This change occurs particularly happens around the head and neck. Ultimately, this is a common goal for weight loss. It looks “healthier” and “thinner.” These changes can also help with breathing problems, like sleep apnea.
However, if teeth aren’t properly cared for, occlusal stability may be at risk. It might not seem urgent now, but it’s a key point to think about for the future. Increased decay risk equates to a larger likelihood of loosing a tooth. The tooth loss will impact chewing, and the facial structures end up sagging and dropping. Most everyone can see this is the traditional “old-person” face. Think about your grandma or grandpa who are missing their teeth and have dentures.
The timeline for these changes varies. Some patients feel hardly any effects. Others, however, may face serious problems if the decay is allowed to worsen.

Some ozempic dental considerations are – if the decay causes significant tooth loss, it will effect how “old” a person looks.
What should I do about Ozempic Dental Side Effects?
Advice #1 – TELL YOUR DENTIST
Obviously, this was written by a dentist to help with the cross effects of teeth. So it is natural to encourage communication with your dentist. As a dental professional I often am told that “it has nothing to do with dentistry”, but this is false. Letting your dentist know all of your medications will help them considerably. In particular here, it is important to tell your dentist when you started (or plan to start) Ozempic. Also helpful is the dosage, duration, and any observed side effects, especially dry mouth.
Advice #2 – Supplements and Dietary Changes
Managing dry mouth is tough. Even the best strategies offer limited help. And, admittedly, it is disheartening to not have a solution when my patients want relief. Lozenges aren’t as helpful as you might think. Also, medical prescriptions don’t provide as much relief as we hope. That said, some tips and tricks have been helpful in the long run. Here are some evidence-based suggestions:
-
Use xylitol-based gum or mints to boost saliva and fight cavity-causing bacteria.
-
Drink plenty of water, aiming for 2-3 liters daily if you have a dry mouth.
-
Try specialized mouth rinses like Biotène or CloSys for comfort.
-
Zinc and vitamin D supplements may help.
-
Oral probiotic can support healthy bacteria in the mouth.
Advice #3 – Is there an alternative? Ask the doctor.
Unfortunately, people cannot do much to reverse the cause of age-related dry mouth. This is not true with medically induced dry mouth. Managing medication-induced dry mouth is challenging. Sometimes, the best solution is to change or stop the medication. This needs coordination with your dentist and doctor.
While less common, there may be other medical or lifestyle solutions that can help. The only way to eliminate medically induced dry mouth completely is to stop the drug. That said, there are different GLP-1 receptor agonists. And their effect may not be as well known. They do affect oral health in various ways.
For completeness’ sake, a healthcare provider may suggest the following medications.
Ozempic (semaglutide) often causes dry mouth, nausea, and vomiting. These side effects can lead to oral problems. As we talked about, its strong appetite suppression can cause nutritional deficiencies. This may harm oral health.
Wegovy is chemically similar to Ozempic but at a higher dose. It often causes worse nausea and dehydration in weight loss patients. This leads to more dry mouth than Ozempic used for diabetes.
Trulicity (dulaglutide) has a milder gastrointestinal effects with fewer reports of nausea. This translates to less pronounced issues, unless compounded by advanced diabetes.
Mounjaro (tirzepatide) is a newer dual GIP/GLP-1 agonist. It can cause dry mouth just as much as, or even more than, Ozempic. This is especially true if the dosage increases quickly.
What to do moving forward: My typical protocols for patients with these issues.
For patients on long-term GLP-1 therapy with ozempic dental side effects, I usually suggest a clear monitoring plan:
-
In the first three months:
-
Check the baseline salivary flow.
-
Do a complete dental and oral-facial exam.
-
Reinforce oral hygiene instructions.
-
Introduction of a high-fluoride toothpaste.
-
Put in place saliva stimulation strategies and educate patients about self-monitoring.
(While you may be used to 6 months or even a year between visits, it is wise to schedule more frequent follow-ups.)
-
-
From three to six months:
-
Perform periodontal charting, plaque evaluations, and check for fungal infections.
-
Check if prescriptions or fluoride trays are needed for severe cases.
-
-
Between six and twelve months,
-
Conduct another full exams,
-
Perhaps take comparison photos,
-
Consider remineralizing agents (hydroxyapatate applications) for early demineralization.
-
-
Beyond twelve months,
-
Conduct comprehensive periodontal evaluations on a regular basis. ,
-
Check areas that are difficult to brush more closely.
-
Possibly adjust recall frequency to 3-4 times yearly for high-risk patients.
-
If using it for a long time leads to issues, the dentist should talk to the doctor who prescribed it.
-
More Questions? Comment or call! Book your appointment now!
It’s essential to work closely with the prescribing physician when considering Ozempic Dental Side Effects, especially for off-label use of Ozempic for weight loss Ultimately, the goal is to help patients reach their health goals without compromising oral health. We addressed that problems worsen when patients use the medication without necessary lifestyle changes. This leads to ongoing dry mouth with no relief in sight.
Balancing the benefits of GLP-1 agonists with their oral health risks requires collaboration between dental and medical teams. Educating patients about potential oral side effects should happen before starting therapy. Proactive prevention strategies should begin immediately.
For those already facing issues, a team approach focusing on symptom management and possible medication adjustments offers the best outcome. If you are in need of further advice or would like a personalized plan, contact us and we would love to help you!
— Dr. Bradly Mouritsen DMD
King Benjamin Dental
Naples, FL

Dr. Bradly Mouritsen, founder of King Benjamin Dental in Naples, FL — delivering personalized, patient-first care rooted in excellence, precision, and passion.